Published on: 09/09/19
The National Paediatric Brain Injury Conference 2019 run by The Children’s Trust took place on Friday asking ‘where do we go from here?’. We share lessons learnt.
Published on: 09/09/19
The conference took a visionary look at paediatric acquired brain injury (ABI), exploring what the future might hold.
Topics ranged from the political agenda to latest research and interventions – with speakers providing new insight for the 200+ professional delegates attending.
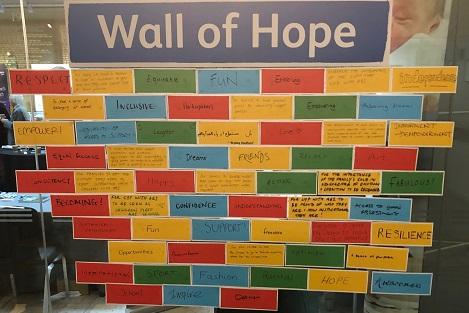
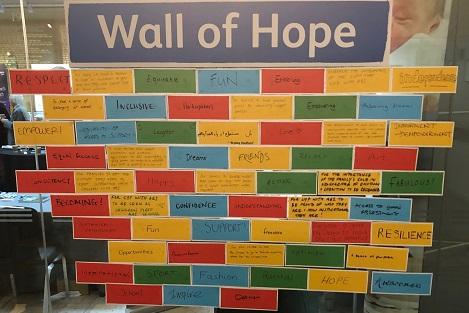
The conference was chaired by Dr Charlie Fairhurst, Consultant Paediatric Neurodisability and Head of Paediatric Neurosceience, Evelina London Children’s Hospital, and sponsored by Irwin Mitchell. Delegates filled a Wall of Hope in between sessions, which symbolised collective aspirations for the future for children with brain injury.
The Wall was built with the words ‘inclusive’, ‘dreams’, ‘independence’ and ‘resilience’, and messages included ‘For children and young people with ABI to been seen as children first, ABI second’.
Here’s the lowdown on the topics of the day – with key findings and lessons learnt...
First to take the stage was Dr Andrew Bateman, Chair of United Kingdom Acquired Brain Injury Forum (UKABIF). UKABIF produced 2018’s Time for Change report outlining the critical role of neurorehabilitation in the ABI care pathway and the role of Rehabilitation Prescriptions.
Andrew spoke about engaging politicians on the topic of ABI, mentioning the progress made and key role played by Chris Bryant MP. He cited how the government will soon be moving on and thinking about policies and the landscape going forward, and how parties will be working on their manifestos.
Andrew asked how many of the audience had contacted their MP this year – then specifically on brain injury. He encouraged further action saying: “We can actually influence policy and influence and change the landscape for people with brain injury by working with those who work for us – elected representatives.”
The need to lobby was reiterated and Andrew added: “People don’t ‘get’ that invisible disability matters. Until we get policy change that it’s a ‘right’ for people to have the rehabilitation, we have to keep up the pressure.”
The inspirational Charlie Fogarty MBE, who was hit by a car in 2012 as a teenager, shared his journey with delegates explaining how, after an ABI, you have got to ‘believe in yourself, have a good support network and not let your injury define you’.
Thoroughly entertaining the audience with his wit and humour Charlie talked about his life before the accident, and how he was on his way to become a professional footballer, through to being a patient at Birmingham Children’s Hospital then rehabilitation at The Children’s Trust.
Over five years on, Charlie is playing football all over the world and is a motivational speaker. He credits parental and family support in everything he’s done and a ‘never give-up’ attitude.
“Remember that the doctors didn’t think I would finish my education, but my story just shows that anything is possible with self-belief, determination and a lot of hard work,” said Charlie.
Dr Suzanna Watson, Consultant Clinical Psychologist, Lead for Neuropsychology Services, Cambridge and Peterborough NHS Foundation Trust, explained how, as professionals, the audience only see a snapshot of a child at a particular time post ABI, whether it’s in acute care, on the ward or in the community.
Suzanna conveyed how there is a greater need to think about children long-term, and how it is essential to get commissioners to think about long-term needs to ensure a child has the best outcomes.
The pioneering community neurorehabilitation model being used in the East of England (the CCPNR service) was explained. Suzanna said: “Early specialist intervention changes the trajectory of their [the child’s] recovery after a brain injury.”
Areas that matter most to children and young people with ABI were cited, including school and education, emotional functioning, and support and relationships.
Suzanna described participation as the most important need for children within goal setting. Without participation, and key people in a child’s life identifying their needs, the gap between a child and their peers can increase over time, with social and economic consequences.
The NHS long-term plan (January 2019) was cited as ‘a great opportunity to bring ABI in children onto the agenda’. Suzanna concluded that commissioners should be alerted early in the pathway and to help them understand the life-long nature of ABI.

“There is currently no validated assessment for children and young people and that needs to be addressed,” said Dr Karen Elliott, Director of Gill-Thwaites & Elliott Consultants. The consultancy developed the SMART investigative and diagnostic tool, which is used for adult patients to ensure people in a prolonged disorders of consciousness get a standardised assessment.
The benefits of using an assessment tool were covered with further validation of the tool for children and young people as the next step. Dr Helen Gill-Thwaites MBE, Director, concluded: “Whatever assessment we use we need to involve the family.”
Social impairment is a major determinant for quality of life, said Professor Vicki Anderson, Paediatric Neuropsychologist and Director of Clinical Sciences Research at Murdoch Children’s Research Institute, Australia. She explained how social impairment impacts 6/10 children post brain injury, while only impacting 1/10 healthy children.
“Social skills development is a really core goal”, said Vicki. She cited research that showed the mismatch between children and parent’s priorities, as children put ‘friends’ as their top priority, while parents put ‘health’.
Despite the potential for social problems after an illness, which can affect outcomes for the long-term, Vicki cited how social problems were ‘hidden’ as they were not a diagnostic category for professionals, unlike anxiety and depression. Considering the child’s long-term social-emotional outcomes is key to help with the child’s peer acceptance and mutual friendships.
Vicki showed how a programme in Australia is helping parents in terms of the child’s social-emotional outcomes. She said: “While we can’t change what happened to the brain we do have an opportunity in terms of the environment.” Vicki explained that ‘we can help families change their behaviour’ and help them deal with the new situation.
Intervention programmes for parents being used in Australia include Signposts for building better behaviour, a cognitive behaviour based therapy programme, and Take a breath group based intervention. Take a breath – ‘Caring for you, caring for your child’ – covers parent mental health and is about accepting life as it is and doing the best you can.
The programmes are being used in clinical practice in Australia, and have been shown to reduce traumatic stress and guilt and worry about the child. Vicki said: “The environment (ie family) offers an opportunity to improve child outcomes, via parent-focused support and intervention”.
The complexities of neuro-imaging were discussed by Dr Kshitij Mankad, Consultant and Neuroradiology Speciality Lead at Great Ormond Street Hospital for Children, who challenged the audience with brain scan images that were not always representative or typical of what a clinician may expect.
Kshitij explained that ‘there is no normal’ and that a scan could show severe brain injury while the child’s everyday life is barely affected. He also showed the challenges of reading scans, for example comparing the presentation of stroke and abusive trauma to the head.
The key message for clinicians was: “Don’t treat the scan. Treat the child.”
Dr Stacy J Suskauer, Director, Brain Injury Clinical Research Center, Kennedy Krieger Institute, presented on the future of assessment in disorders of consciousness. Developments made were presented and Stacy called for further validation of paediatric measures in the assessment of consciousness.
The need for standardised behavioural measures, with larger sample sizes and natural history data, was cited, along with emerging intervention trials with the development of multi-site partnerships.
Stacy added: “Consciousness is complex... No one intervention is going to work for everybody. For all interventions there are some responders and some non-responders and it’s all about finding the right one.”
The Children’s Trust runs the National Paediatric Brain Injury Conference every year with the next conference planned for a Virtual event in February 2021.