Much of what makes us behave as we do is down to our ‘cognitive functions’. Put simply, this is a way of describing the complex things that go on inside our heads.1
These functions are our thought processes, the way we understand language, and the way we plan and make judgements (among other things). It’s also about the way we learn and process information, and the way we concentrate.2, 3
The way in which children process information may be affected. You may hear professionals talking about the way acquired brain injury affects these ‘cognitive functions’.
The way a child organises themselves, the way they remember things, or the control they have over their behaviour may be affected.4 These things might not be immediately recognisable to others – it’s not like breaking a leg and having to wear a cast. And it’s for this reason that acquired brain injury is often called “the hidden disability”.5
A nurse from The Children’s Trust explains how brain injury can sometimes be an ‘invisible’ injury.
Amnesia
Our memory is a complicated system, using different parts of the brain. It is not uncommon for people with acquired brain injury to experience amnesia.6 This is a state where someone is unable to remember particular periods of time, and there are different kinds:
Post-traumatic amnesia: happens immediately after the injury. This is a temporary state, where the person is conscious, but their everyday memory for events and conversations isn’t working as it should.
A child might have well-wishers at the hospital, but forget about the visit shortly afterwards. They may forget a recent meal.
Retrograde amnesia: is when a child can’t remember the time immediately before their injury. This can sometimes stretch back weeks, months or even years. They may not remember the accident itself.
These memories may return over time, but sometimes patches of memory will be permanently lost.7 Memory is often affected in the long term after a brain injury.
Memory
Difficulties with memory are common after an acquired brain injury 8 It's for this reason that we have a dedicated section on memory that includes a number of practical strategies to assist children and their families.
Attention 9
The brain has only a limited amount of capacity to attend to things at any one time. It’s like the processing power of your PC. If you have lots of things going on at the same time, there’s less processing power available. A simpler comparison is with a pie chart as shown below. If you drive, think about your experiences when you first learnt to drive, compared to the way you drive now.
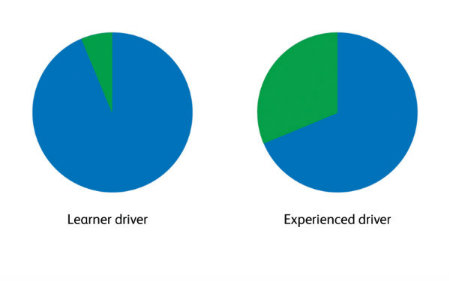 In those early lessons, it took all of your effort and concentration (the blue in the chart). There was only a little bit left to listen to what your instructor was telling you (the green). When you become a more confident driver, less of your attention is used on driving and you are able to give more attention to other things, such as listening to the radio, or talking to a passenger. You are on ‘autopilot’.
In those early lessons, it took all of your effort and concentration (the blue in the chart). There was only a little bit left to listen to what your instructor was telling you (the green). When you become a more confident driver, less of your attention is used on driving and you are able to give more attention to other things, such as listening to the radio, or talking to a passenger. You are on ‘autopilot’.
If you drive abroad or go on a complicated journey, then the amount of the pie attending to driving changes again.10
The difficulty with acquired brain injury is that some of the things a child previously did on ‘autopilot’ are now things they have to think about. They are back at the point you were at in those early driving lessons.
So there isn’t as much capacity left for other things, such as learning in a classroom situation. Children may have difficulty switching between doing different things.11
Difficulty with attention is a good example of how the effects of acquired brain injury are often linked together. Children who struggle to control their attention may become overactive, and may become over-excited easily.11 Children may seem easily distracted. And as with other aspects of acquired brain injury, this may be misunderstood by others as naughtiness.12
Speech and communication
Talking with other people is something most of us take for granted. Yet this is can be a very complex skill,13 using different parts of our brain.
Some children have difficulty with communication after an acquired brain injury. We look at speech and communication in more depth in our dedicated section on ‘talking with children with an acquired brain injury’.
Lack of insight and awareness
Judging our own behaviour is a sophisticated skill which takes place in the frontal lobes of the brain. This part of the brain is particularly prone to injury. 14, 15 And as a consequence, acquired brain injury may affect a child’s self-awareness – their own understanding of who they are and what they’re able to do.16
For some children, this means they may not fully understand or acknowledge what has happened to them.
They may see themselves as no different to the way they were before the injury, which might mean they refuse help.
Some children may set themselves unrealistic goals, or not recognise the mistakes they are making.17 They may need to be given plenty of explanation about what’s happened at a level that works for them.16
Sometimes, this lack of self-awareness can be a positive thing. Children may not be affected by an impact on their self-esteem.18
To make things even more confusing, some children experience an entirely opposite effect to that described above. They may be very much aware of how they have changed.19
This can come with its own problems, in that children may feel anxious or even depressed at what they have lost.20, 21
Something else that goes on in the frontal lobes of our brains is the ability to put ourselves in someone else’s shoes, or empathy.22 Children may say things that seem insensitive or odd 23 to others. This may lead to trouble getting on with friends and family, which in turn can lead to a child feeling isolated.24
Emotions and mental health
The trauma of a brain injury can have an enormous impact on a child’s wellbeing and sense of themselves.25
We naturally associate childhood with happiness and a carefree existence, but some children experience mental health difficulties as a result of their experiences.26
Being away from home and taken to hospital can be stressful enough. Children may be suffering from post-traumatic stress disorder (PTSD) after being at the centre of a medical emergency.27
If the child has been involved in an accident in which others have been hurt or killed, they may be experiencing grief.
These are some of the immediate factors to think about. But there are also important long-term emotional consequences that many children with acquired brain injury and their families deal with.
Let’s go back to some of the key difficulties children with acquired brain injury may experience:
- Loss of abilities 28
- Difficulties communicating with those around them 29
- Tiredness, irritability, not being able to ‘keep up’
- Changes in behaviour 30
It’s easy to see how anyone might struggle as they adjusted to these enormous and often upsetting changes.
Some children may experience frustration, aggression or even depression as they come to realise that they have lost the ability to do things they were able to before.20, 31
They may feel helpless because they are not as independent as they have been in the past, or the brain injury may have changed their role within the family.32
Children may feel frustrated and may experience a sense of loss as they struggle to do things they’ve been able to do before.28
Being away from friends and the normality of school life can make things difficult for children. They may not be able to go out and play and may feel they’re ‘missing out’.33, 34
When they return to school, a child might be anxious about how well they will cope. They might be anxious about keeping up with schoolwork, or getting back into the flow of school-life.
Their injury may make it hard for them to feel they ‘fit in’, which might lead to anxieties. It may be hard for them to maintain friendships.
Some children experience depression,35 which can be shocking to hear for parents.
If you are at all concerned about your child’s wellbeing, the healthcare professionals around you will be able to point you in the right direction for help.
It’s also worth remembering that any illness doesn’t exist in a vacuum. There may well be other things going on at home that can impact a child’s emotional wellbeing. 36
A GP can refer children to the local CAMHS – Child and Adolescent Mental Health Services.
Building a support network for you and your child will benefit their wellbeing and emotional health.


